Orthopedic Surgery and Sports Medicine
Right Here, Close to Home!
Orthopedic Surgery
Orthopedics focuses on injuries and diseases of the body’s musculoskeletal system. This complex system includes bones, joints, ligaments, tendons, muscles and nerves. Orthopedics includes care for patients of all ages – from newborns to young athletes to individuals in their golden years.
What is an Orthopedic Surgeon?
Often called orthopedists, orthopedic surgeons are medical doctors with training in the proper diagnosis and treatment of injuries and diseases of the musculoskeletal system. Most orthopedic surgeons complete up to 14 years of education.

Orthopedic surgeons manage:
offers the following orthopedic procedures & services:
In an arthroscopic examination, a small incision is made in the patient’s skin with a pencil-sized instrument that contains a small lens and lighting system. This is used to magnify and illuminate the structures inside the joint. By attaching the arthroscope to a miniature television camera, the surgeon is able to see the interior of the joint through this very small incision rather than a large incision.
The camera attached to the arthroscope displays the image of the joint on a television screen, allowing the surgeon to look, for example, throughout the knee at cartilage and ligaments, and under the kneecap. The surgeon can determine the amount or type of injury, and then repair or correct the problem, if it is necessary.
The most commonly performed joint replacements are knee and hip replacements, which assist in alleviating pain and restoring function in severely damaged joints. The surgical procedure for both involves replacing the damaged bone with an artificial joint, also known as a prosthesis; this is usually done when other treatment options have failed to significantly provide relief to the damaged area.
The following links will provide you with more information related to knee and hip replacements:
The anterior cruciate ligament (ACL) is one of the main stabilizing ligaments in the knee. A tear of the ligament can be partial or complete. It is a serious injury leading to destabilization of the knee. Non-surgical treatment of a chronic tear depends on the patient’s age and needs. The low demand or unathletic person may be content to decrease activities so that the knee never gives way. More athletic individuals may be able to cope by wearing a brace to stabilize the knee during sports.
Open reduction is a manipulation of a fractured bone; this occurs by making an incision in the skin and muscle over the site of the fracture. Whereas, internal fixation is a surgical procedure that stabilizes and joins the ends of fractured (broken) bones by mechanical devices such as metal plates, pins, rods, wires, or screws.
Carpal tunnel syndrome can be caused by compression of the median nerve at the wrist, which can lead to pain and weakness in the hand. The median nerve supplies sensation to the thumb, first two fingers, part of the third finger, and also to some of the muscles of the hand. Carpal tunnel surgery involves 1 or 2 small incisions over the palm of the hand. The surgery can be performed endoscopically (using a small camera attached to a monitor). The carpal ligament is located directly below the incision(s), in the area of the palm, just past the wrist on the palm, and in the direction of the fingers (distal).
Trigger finger is a condition in which one of your fingers or your thumb catches in a bent position. Your finger or thumb may straighten with a snap – like a trigger being pulled and released. If trigger finger is severe, your finger may become locked in a bent position. Treatment varies. Mild symptoms may improve simply by resting the affected hand and preventing overuse of the problem finger. Nonsteroidal anti-inflammatory drugs can help reduce inflammation and swelling. More serious cases may require injections of steroid medication or surgery.
Tennis Elbow is a degenerative condition of the tendon fibers that attach on the bony prominence (epicondyle) on the outside (lateral side) of the elbow. The tendons involved are responsible for anchoring the muscles that extend or lift the wrist and hand. In most cases, non-operative treatment should be tried before surgery. If symptoms do not improve the next step is a corticosteroid injection around the outside of the elbow. This can be very helpful in reducing pain. Physical therapy may be recommended and can help complete recovery.
Surgery is considered only in patients who have incapacitating pain that does not get better after at least six months of non-operative treatment. The surgical procedure involves removing diseased tendon tissue and reattaching normal tendon tissue to bone. The procedure is an outpatient surgery; you do not need to stay in the hospital overnight. It can be performed under regional or general anesthesia.
This surgical procedure involves relocating the ulnar nerve, which runs from the arm to the finger tips, to an alternate location in the general vicinity of its original location. If the nerve has become compressed, patients may be experiencing frequent numbness and discomfort.
Troy Regional now offering innovative technology in total knee replacement with Stryker Mako SmartRobotics
Troy Regional Medical Center is excited to offer Mako SmartRobotics. This advancement in joint replacement surgery offers an innovative approach to total and partial knee replacements and transforms the way total knee replacements are performed by Dr. Robert Liljeberg, Board Certified Orthopedic Surgeon.
“With the Mako Total Knee Replacement, I know more about my patients than ever before and I’m able to cut less. For some patients, this can mean less soft tissue damage; for others, greater bone preservation,” Dr. Liljeberg said. “Mako’s 3D CT allows me to create a personalized plan based on each patient’s unique anatomy all before entering the operating room. During surgery, I can validate that plan and make any necessary adjustments while guiding the robotic arm to execute that plan. It’s exciting to be able to offer this transformative technology across the joint replacement service line to perform total knee and partial knee replacements.”
“We are proud to offer this highly advanced robotic technology in our service area,” Rick Smith, Troy Regional Chief Executive Officer, said. “This addition to our orthopedic service line further demonstrates our commitment to provide the community with remarkable healthcare.”
Mako SmartRobotics™
We understand that knowing what to expect from your joint replacement experience is important to you. As you are reading through this material, please reach out to us to discuss if you have additional questions.
Each patient is unique and can experience joint pain for different reasons. It’s important to talk to us about the reason for your joint pain so you can understand the treatment options available to you. Pain from arthritis and joint degeneration can be constant or come and go, occur with movement or after a period of rest, or be located in one spot or many parts of the body. It is common for patients to try medication and other conservative treatments to treat their knee or hip pain. If you haven’t experienced adequate relief with those treatment options, you may be a candidate for Mako SmartRobotics™ for Total Knee, Total Hip, or Partial Knee replacement.

How Mako SmartRobotics™ works
Mako SmartRobotics™ is an innovative solution for many suffering from painful arthritis of the knee or hip. Mako uses 3D CT-based planning software so your surgeon can know more about your anatomy to create a personalized joint replacement surgical plan. This 3D model is used to preplan and assist your surgeon in performing your joint replacement procedure.
In the operating room, your surgeon follows your personalized surgical plan while preparing the bone for the implant. The surgeon guides Mako’s robotic arm within the predefined area, and Mako’s AccuStop™ technology helps the surgeon stay within the planned boundaries that were defined when the personalized preoperative plan was created. By guiding your doctor during surgery, Mako’s AccuStop™ technology allows your surgeon to cut less by cutting precisely what’s planned1-3 to help protect your healthy bone.4-8
It’s important to understand that the surgery is performed by an orthopedic surgeon, who guides Mako’s robotic arm during the surgery to position the implant in the knee and hip joints. Mako SmartRobotics™ does not perform surgery, make decisions on its own or move without the surgeon guiding it. Mako SmartRobotics™ also allows your surgeon to make adjustments to your plan during surgery as needed.
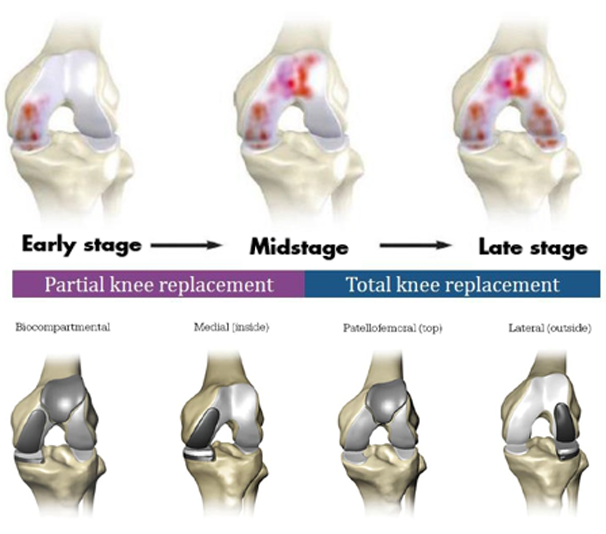
Total Knee vs. Partial Knee Replacement
Based on the severity of the arthritis in the knee, total or partial knee replacement may be recommended by a surgeon. Both procedures involve the orthopedic surgeon guiding Mako’s robotic arm to remove diseased bone and cartilage.
- Mako SmartRobotics™ for Partial Knee replacement is a treatment option for adults living with early- to midstage osteoarthritis (OA) that has not yet progressed to all three compartments of the knee. Depending on where the arthritis affects the knee, patients may have an implant inserted in any of the following areas:
- In a unicondylar knee replacement, only one area (or compartment) of the joint is replaced.
- A patellofemoral knee replacement replaces the kneecap (or patella) and the grove at the lower end of the thighbone (or femur).
- A bicompartmental knee replacement affects two compartments of the knee – the inside (medial) and knee cap.
- In comparison, Mako SmartRobotics™ for Total Knee replacement is a treatment option for adults living with mid- to late-stage osteoarthritis of the knee. With a Mako Total Knee replacement, the entire knee joint is replaced, and the surgeon inserts a Triathlon Total Knee implant. With over a decade of clinical history, Triathlon knee replacements are different than traditional knee replacements because they are designed to work with the body to promote natural-like circular motion.9-11
- Mako SmartRobotics™ for Total Hip replacement is intended for patients who suffer from noninflammatory or inflammatory degenerative joint disease (DJD). Some forms of DJD include osteoarthritis (OA), post-traumatic arthritis, rheumatoid arthritis (RA), avascular necrosis (AVN) and hip dysplasia.
IMPORTANT INFORMATION
Knee & hip replacements
Knee and hip replacement is intended for use in individuals with joint disease resulting from degenerative and rheumatoid arthritis, avascular necrosis, fracture of the neck of the femur or functional deformity of the hip.
Knee joint replacement is intended for use in individuals with joint disease resulting from degenerative, rheumatoid and post- traumatic arthritis, and for moderate deformity of the knee.
Joint replacement surgery is not appropriate for patients with certain types of infections, any mental or neuromuscular disorder which would create an unacceptable risk of prosthesis instability, prosthesis fixation failure or complications in postoperative care, compromised bone stock, skeletal immaturity, severe instability of the joint, or excessive body weight.
Like any surgery, joint replacement surgery has serious risks which include, but are not limited to, pain, infection, bone fracture, change in the treated leg length (hip), joint stiffness, hip joint fusion, amputation, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis (blood clots in the legs)), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus (loss of intestinal digestive movement)), vascular disorders (including thrombus (blood clots), blood loss, or changes in blood pressure or heart rhythm), bronchopulmonary disorders (including emboli, stroke or pneumonia), heart attack, and death.
Implant related risks which may lead to a revision of the implant include dislocation, loosening, fracture, nerve damage, heterotopic bone formation (abnormal bone growth in tissue), wear of the implant, metal and/or foreign body sensitivity, soft tissue imbalance, osteolysis (localized progressive bone loss), audible sounds during motion, reaction to particle debris , and reaction to metal ions (ALTR). Knee and hip implants may not provide the same feel or performance characteristics experienced with a normal healthy joint.
The information presented is for educational purposes only. Speak to your doctor to decide if joint replacement surgery is appropriate for you. Individual results vary and not all patients will return to the same activity level. The lifetime of any joint replacement is limited and depends on several factors like patient weight and activity level. Your doctor will counsel you about strategies to potentially prolong the lifetime of the device, including avoiding high-impact activities, such as running, as well as maintaining a healthy weight. It is important to closely follow your doctor’s instructions regarding post-surgery activity, treatment and follow-up care. Ask your doctor if a joint replacement is right for you.
Stryker Corporation or its other divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: AccuStop, Mako, SmartRobotics, Stryker, Triathlon. All other trademarks are trademarks of their respective owners.
References
- Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016;98(8):627-635. doi:10.2106/JBJS.15.00664
- Illgen RL, Bukowski BR, Abiola R, et al. Robotic-assisted total hip arthroplasty: outcomes at minimum two year follow up. Surg Technol Int. 2017;30:365-372.
- Mahoney O, Kinsey T, Mont M, Hozack W, Orozco F, Chen A. Can computer generated 3D bone models improve the accuracy of total knee component placement compared to manual instrumentation? A prospective multi-center evaluation. Poster presented at: 32nd Annual Congress of the International Society for Technology in Arthroplasty; October 2-5, 2019; Toronto, Canada.
- Suarez-Ahedo C, Gui C, Martin TJ, Chandrasekaran S, Lodhia P, Domb BG. Robotic-arm assisted total hip arthroplasty results in smaller acetabular cup size in relation to the femoral head size: a matched-pair controlled study. Hip Int. 2017;27(2):147-152. doi:10.5301/hipint.5000418
- Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty. 2018;33(8):2496-2501. doi:10.1016/j.arth.2018.03.042
- Hozack WJ. Multicentre analysis of outcomes after robotic-arm assisted total knee arthroplasty. Bone Joint J:Orthop Proc. 2018;100-B(Supp_12):38.
- Banks SA. Haptic robotics enable a systems approach to design of a minimally invasive modular knee arthroplasty. Am J Orthop (Belle Mead NJ0. 2009;38(2 Suppl):23-27.
- Hampp E, Chang TC, Pearle A. Robotic partial knee arthroplasty demonstrated greater bone preservation compared to robotic total knee arthroplasty. Poster presented at: Orthopaedic Research Society Annual Meeting; February 2-5, 2019; Austin, TX.
- Piazza S. Designed to maintain collateral ligament stability throughout the range of motion. Stryker-Initiated Dynamic Computer Simulations of Passive ROM and Oxford Rig Test. 2003.
- Wang H, Simpson KJ, Ferrara MS, Chamnongkich S, Kinsey T, Mahoney OM. Biomechanical differences exhibited during sit-to-stand between total knee arthroplasty designs of varying radii. J Arthroplasty. 2006;21(8):1193-1199. doi:10.1016/j.arth.2006.02.172
- Gómez-Barrena E, Fernandez-García C, Fernandez-Bravo A, Cutillas-Ruiz R, Bermejo-Fernandez G. Functional performance with a single-radius femoral design total knee arthroplasty. Clin Orthop Relat Res. 2010;468(5):1214-1220. doi:10.1007/s11999-009-1190-2
MKOHMT-PE-3_Rev-2_24739
Copyright © 2020 Stryker